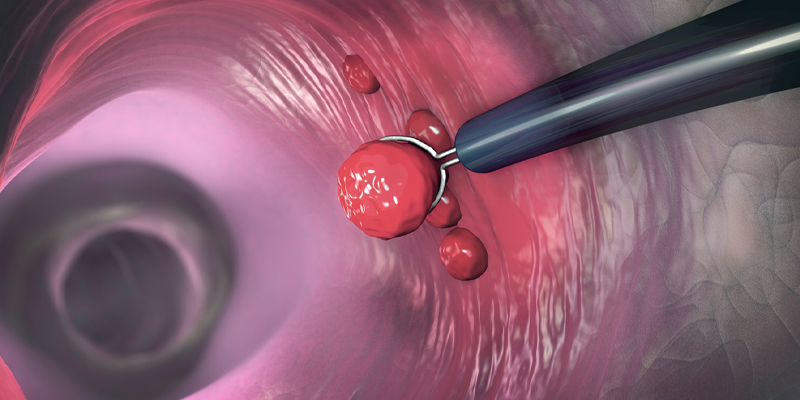
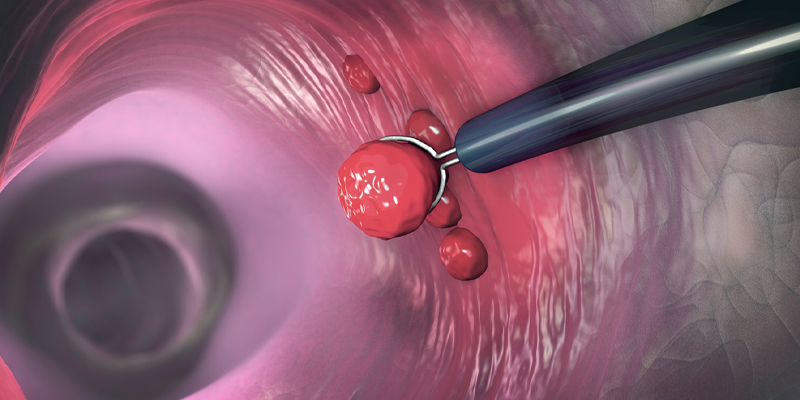
A colonoscope is a fiberoptic tube containing a image collecting chip that can show the inside of colon and the end of the small bowel for cancer screening purposes and diagnosis of other diseases like diarrhea or bleeding. This 5 foot long tube has the ability to transmit light, flush the colon with water, and has a channel to allow for biopsy of lesions, removal of polyps with snare or small pinchers/forceps or even injection of drugs/tattoos and cautery of bleeding sites.
Colonoscopy is a safe and effective tool that is much more accurate than x-ray evaluations of the GI tract, and allows for potential treatment of lesions during the examination. The procedure saves lives by removing polyps that could grow into colon cancer later.
The American Cancer Society guidelines changed in 2020 to come in line with a number of other organizations in recommending the start regular screening of colon cancer should now begin at age 45 for average adults.
Screening for colon cancer for people in good health with a life expectancy of more than 10 years should be done up to age 75. The decision to screen individuals 76 through age 85 needs to be based on overall health/life expectancy, prior lesions found on screening, and personal preferences of the patient. Individuals 86 and older can get colonoscopy for diagnostic purposes but are not generally candidates for screening.
A patient is NOT considered routine risk for colon cancer screening if they have any of the following:
The key factor in a successful colonoscopy is how clean the bowel is at the time of the procedure. To see polyps and other lesions, the colon MUST be very clean. This also decreases the time of the procedure, and decreases the chances you might have to be brought back sooner for “inadequate visualization”. Rarely the prep is so poor the patient has to reprep to bring them back the next day to repeat the exam.
A clear liquid diet should be used for the day prior to the exam. This includes broth, water, sport drinks (no red or purple), no-pulp popsicles, jello, black coffee and sodas. Your doctor may recommend additional days of clear liquids if you have severe constipation.
A bowel prep will be used the day prior to procedure. A split preparation is likely to be advised by your doctor with second half of the prep completed at least 6 hours prior to your procedure time. These split dose preps are associated with the best visualization of the colon in many studies but more difficult/confusing in terms of steps. It will be worth it!
The type of purgative or bowel prep will be determined by your doctor based on your medical history. Average patients may get a Miralax-based prep, but if you have a cardiac history, renal insufficiency, liver disease or other severe medical condition you may be given another prep for safety. Golytely and other preps are specially designed to reduce fluid/electrolyte shifts in the body—they work by flushing out the stool without pulling in water.
Blood thinners and other medication (like insulin) may need to stopped or adjusted prior to the procedure. Make sure your gastroenterologist is aware of all your medications. If blood thinners other than aspirin are not stopped there is a higher risk of post-polypectomy bleeding.
Your instructions should contain details on where to go for your procedure (hospital or ambulatory surgery center), how to prep, and to bring a driver who can take you home afterwards.
When you arrive, you will get registered, change into a gown to protect your clothing, and an IV will be inserted to give you medication for the procedure. Vital signs for blood pressure, pulse and oxygen saturation will be taken throughout the process.
You will be asked to lay on your left side down and bring your knees up. A medication will be given, sometimes with a slight burning or metallic taste, and you will be ready for the procedure.
The colonoscope is gently inserted and advanced through the rectum, remaining colon up to the cecum and sometimes into the end of the small bowel/terminal ileum.
The vast majority of people sleep until they are back in the recovery room, ready to hear the findings of the procedure. Sometimes, although talking, they have little recollection of the conversation. This is why it is helpful to have a second person listening to the discussion. This fogginess is much less common with propofol as a sedative than with versed we used previously.
We do suggest eating a light meal of your usual diet after the procedure. Don’t be alarmed at the amount of air expelled; this is natural and will make you more comfortable.
Colonoscopy is safe and effective, but complications can rarely occur.
REMEMBER to tell your physician and anesthesia support staff if you are pregnant or have any allergies to medications to make this test as safe as possible.
You will be given post procedure instructions to monitor for abdominal pain, fevers, and chills. Eat lightly and expel the gas. Light housework/activity is ok, but we would advise waiting until the following day to return to work.
The nursing staff will likely contact you the following business day to check on you and answer any questions you may have. Your physician’s office will contact you with any pathology results that were obtained at the time of the procedure. This can be helpful as the type of polyp and size will likely be factors in determining how soon you need to return for repeat colonoscopy. If there were no polyps and a negative family history of colon cancer/polyps then rescreen after a good prep is usually 10 years!
You and Colonoscopy—this is a great multimedia site with multiple animations for teaching: http://youandcolonoscopy.com/en-cln/home
Web MD contribution: https://www.webmd.com/colorectal-cancer/colonoscopy-what-you-need-know
©2024 Copyright | Website Privacy Policy | Digital Marketing by Authority Solutions®